Urethral Stricture & Reconstruction
Urethral stricture is a term used to describe a blockage in the urethra.
How does the urinary system work?
The urinary tract begins with the kidneys. The kidneys, one on each side, sit high in the upper abdomen partially underneath the rib cage. They filter the blood to extract excess waste products and fluid to form the urine. Urine, once formed in the kidneys, travels through a tube on each side, the ureter, down to the bladder. Urine is constantly being made by the kidneys and transported through the ureters into the bladder.
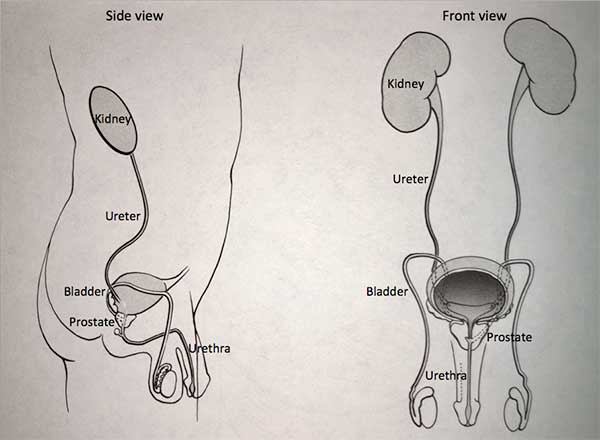
The bladder stores urine until full and then empties to the outside through the urethra. The prostate, which is a gland that is part of the reproductive system, forms the first part of the urethra.
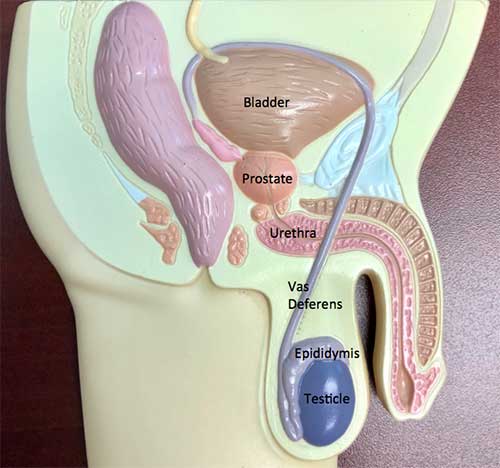
What is the prostate?
The prostate gland makes some of the semen, the fluid which is released during ejaculation. The prostate gland in adults remains a constant size until approximately age 40, when it begins to enlarge. The cause of the enlargement is unknown. Although prostate enlargement does not produce trouble in all men, it may cause obstruction of the urinary pathway in some men.
What Is urethral stricture?
A stricture is a narrowed segment in urethra, the urinary pathway. Normally, during voiding, the urethra is as wide as the caliber of a pen or pencil. When there’s a narrowed segment, the width (opening) of the narrowed segment may be no wider than the tip of the pencil.
What causes a urethral stricture to form?
A urethral stricture may form for a variety of reasons, some of which include congenital conditions (a disorder already present at birth), infection or inflammation, trauma, (which can include injury to the perineum, the area between the scrotum and the rectum, such as may occur if there’s a fall onto a bike seat or a fence) or prior urinary tract surgery or urinary catheterization.
What are the symptoms of urethral stricture?
The urethral stricture causes trouble when it restricts the flow of urine out of the bladder. As the urethral stricture obstructs, it blocks the urinary channel. The bladder then has to work harder to overcome this increased resistance to urine flow. If the blockage is severe enough, the bladder may be unable to empty, leading to a condition called urinary retention. The onset of symptoms of urethral stricture can be very gradual. Symptoms may include difficulty starting the flow of urine, decreased force of urination, and dribbling at the end of urination. There may be incomplete emptying of the bladder which produces a sense of still feeling full even after attempting to pass the urine. Incomplete bladder emptying also leads to “double voiding” in which a man passes the urine and then has to urinate again within a period of 10 to 20 minutes. Other symptoms include the need to pass urine more frequently than normal and the development of a sense of urgency, which is the need to pass the urine as soon as the urge is felt. Urethral strictures may cause hematuria (blood in the urine), urinary tract infection, or there may be some blood spotting from the tip of the penis.
How Is urethral stricture diagnosed?
The most common way to diagnose urethral stricture is with cystoscopy. Cystoscopy refers to the visual inspection of the urethra and bladder. This is carried out by inserting a small fiberoptic catheter into the urethra which allows direct examination. This is typically carried out under local anesthetic in an examination room in the office.
In some cases, an imaging (x-ray) study called a voiding cystourethrogram (VCUG) may be carried out. Contrast is placed into the bladder and images are obtained during voiding to provide a picture of the urethra including the strictured segment.
Why should a urethral stricture be treated?
There are multiple indications for the treatment of urethral stricture. One of the foremost is urinary retention, which is the inability of the bladder to empty any urine. Intervention should be carried out because the stricture impairs drainage of urine out of the bladder which can then cause a large post-void residual (urine left behind after voiding). This residual urine can block the drainage of the kidneys and lead to inadequate kidney function. A bladder sonogram or scan may be done to make sure the residual urine volume is not too high. Severe bleeding or recurrent urinary tract infections are also reasons to proceed with intervention.
What are the treatments for urethral stricture?
Treatment for urethral stricture depends on the length and the location of the stricture. In general, the different types of treatment can be divided into two categories – endoscopic treatment and open surgical procedures. Endoscopic techniques, which are those done with a cystoscope, include balloon dilation and direct vision internal urethrotomy (DVIU). For balloon dilation, a balloon is placed through the narrowed segment and then inflated to expand the narrowed segment of the urethra back to the normal caliber.
A postop catheter (tube to drain urine out of the bladder) is typically not required. With direct vision internal urethrotomy, the strictured segment is incised, with a cystoscopic scalpel or a laser, to open up the narrowed segment.
A catheter is often placed for several days postoperatively. Hazards of these procedures include the potential for bleeding and infection. With each of these techniques, a subset of men develop recurrent stricture in the future and may require repeat treatment.
Open surgical procedures are directed towards removal of the narrowed segment, followed by a reanastomosis (a joining together) of the unblocked segments of the urethra, the areas before and after the narrowed segment.
Hospital stay may be required, and a catheter is usually placed for 1-2 weeks. With open surgical technique, recurrent stricture is less common compared with endoscopic techniques. Hazards may include potential bleeding, infection and, in some men, erectile dysfunction (ED).
In some men, even with one of the above types of intervention, urethral stricture may be an ongoing problem. Management strategies include ongoing office follow-up for office-based cystoscopic dilation, or intermittent patient self-catheterization. With intermittent self-catheterization, the patient passes a catheter at periodic intervals, which helps dilate the strictured segment and keep the urethra open on an ongoing basis.
Overall, urethral stricture is a common urologic condition and one that can be addressed to prevent more severe problems from developing.
Urethral Reconstruction
Urethroplasty
When there is either extrinsic or intrinsic trauma to the urethra, a “scar” forms in the tissue surrounding the urethra. Once this occurs there is a circumferential stricture which impedes the flow of urine. As the stricture tightens, the flow gets slower until the urine is completely blocked. Typically, a urethral dilation will adequately treat 95% of strictures; however, some strictures are dense and dilation will not keep the urethral segment open. A urethroplasty is performed in this situation. During the surgery, the surgeon completely excises the strictured segment and if the stricture is < 2 cm then a Primary repair is performed “Bringing the 2 ends together.” If the stricture is > 2 cm, the ends are too far apart and therefore an interposition graft or a patch is performed to “bridge” the gap between the two ends. Risks of a urethroplasty include infection, bleeding, positional nerve injury, erectile dysfunction and recurrent strictures. The typical “cure” rate is 95%.
Hypospadias
Hypospadias is a congenital disorder of the male urethra, and varies in severity. Hypospadias is when the urethral opening is more proximal on the penis than in the usual position at the head of the penis. This happens during the embryologic development of the penis. The cause of this defect is the failure of the tissue to fully wrap in front of the penis to cover the urethra. Therefore there can be varying degrees of the defect. The more proximal the opening on the penis, the more severe the defect, hence harder to repair.
To repair a hypospadias, local tissue flaps are required. Most hypospadia procedures are performed before the age of 1. Surgical complications include urethral fistula, stricture, and diverticulum formation.
Print PageContact us to request an appointment or ask a question. We're here for you.




