Robotic Sacroculpopexy for Pelvic Organ Prolapse
What Is Pelvic organ prolapse?
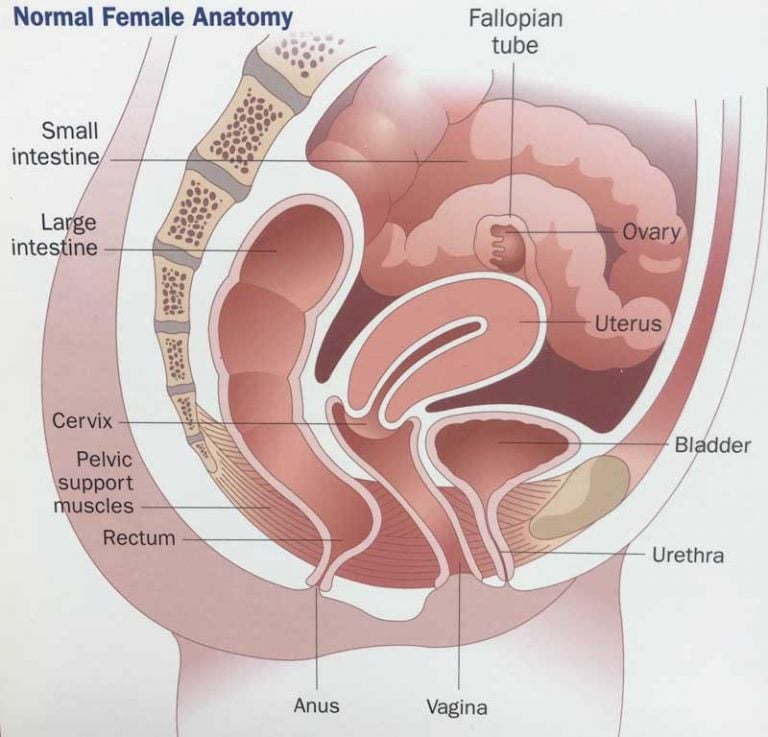
Pelvic organ prolapse occurs when a pelvic organ, such as your bladder, drops (prolapses) from its normal spot in your lower belly and pushes against the walls of your vagina. This can happen when the muscles that hold your pelvic organs in place get weak or stretched from childbirth or surgery.
Many women will have some kind of pelvic organ prolapse. It can be uncomfortable or painful. But it isn’t usually a big health problem. It doesn’t always get worse. And in some women, it can get better with time.
More than one pelvic organ can prolapse at the same time. Organs that can be involved when you have pelvic prolapse include the:
- Bladder (cystocele), this is the most common type of pelvic organ prolapse
- Uterus (uterine proplase)
- Vagina (vaginal prolapse), this occurs after hysterectomy
- Rectum (rectocele)
- Urethra – tube that brings urine from the bladder to the outside of the body (urethral prolapse)
- Small bowel (enterocele)
What causes pelvic organ prolapse?
Pelvic organ prolapse can be made worse by anything that puts pressure on your belly.
Pregnancy and childbirth – Normally your pelvic organs are kept in place by the muscles and tissues in your lower belly. During childbirth these muscles can get weak or stretched. If they don’t recover, they can’t support your pelvic organs. The more times you have been pregnant and the larger the babies, the greater the risk for pelvic organ prolapse.
Hysterectomy – You may also get pelvic organ prolapse if you have surgery to remove your uterus. Removing the uterus can sometimes leave other organs in the pelvis with less support.
Age - The risk of prolapse increases with age. After menopause, there is less estrogen in the vaginal tissues. This can decrease the strength of the tissues.
Family history - Pelvic organ prolapse tends to run in families.
Being very overweight – Having extra weight puts downward pressure on the organs in the lower belly.
Smoking or a long-lasting cough – Smoking or chronic cough (asthma, bronchitis), increases the pressure on the organs in the lower belly.Frequent constipation – Anything that puts pressure on the lower belly can contribute to pelvic organ prolapse over time.
What are the symptoms?
- Pelvic bulge or feeling pressure from pelvic organs pressing against the vaginal wall. This is the most common symptom, seen in 94-100% of patients.
- Feeling as if something is falling out of your vagina
- Feeling very full or pain in your lower belly
- Feeling a pull or stretch in your groin area or pain in your lower back
- Releasing urine without meaning to (incontinence), or needing to urinate a lot
- Having pain in your vagina during sex
- Having problems with your bowels, such as constipation
- Having to manipulate the vagina in order to have a bowel movement or urinate
- Difficulty walking or sitting
How is pelvic organ prolapse diagnosed?
Your doctor will ask questions about your symptoms and about any pregnancies or health problems. Your doctor will also do a physical exam, which will include a pelvic exam.
How is it treated?
Decisions about your treatment will be based on which pelvic organs have prolapsed and how bad your symptoms are.
If your symptoms are mild, you may be able to do things at home to help yourself feel better. You can relieve many of your symptoms by adopting new, healthy habits.
Kegel exercises – Special exercises that make your pelvic muscles stronger
Reach and stay at a healthy weight
Avoid constipation
Avoid lifting heavy things that put stress on your pelvic muscles
Cut back on caffeine, which acts as a diuretic and can cause you to urinate more often
Estrogen cream – If you still have symptoms, vaginal estrogen cream may be prescribed. This improves the health and strength of the pelvic floor. It is applied with your fingertip every night for a week then every night Monday, Wednesday, Friday. Estrogen cream should be avoided or used with caution in women with history of breast, endometrial or other gynecologic cancer, gallbladder problems and history of blood clots (deep venous thrombosis or DVT, pulmonary embolus or PE).
Pessary – You may have you fitted with a device called a pessary to help with the pain and pressure of pelvic organ prolapse. It is a removable device that you put in your vagina. It helps hold the pelvic organs in place. However, if you have a severe prolapse, you may have trouble keeping a pessary in place.
Surgery is another treatment option for serious symptoms of pelvic organ prolapse. Surgery is usually delayed until you are done having children. This is because the strain of childbirth could cause your prolapse to come back.
You may want to consider surgery if:
- You have a lot of discomfort because of the prolapsed organ. You have a problem with your bladder and bowels.
- The prolapse makes it hard for you to enjoy sex.
Types of surgery for Pelvic Organ Prolapse include:
- Surgery to repair the tissue that supports a prolapsed organ.
- Surgery to repair the tissue around your vagina.
- Surgery to close the opening of your vagina.
- Surgery to remove the uterus (hysterectomy).
Pelvic organ prolapse can come back after surgery. Doing Kegel exercises to make your pelvic muscles stronger will help you recover faster from surgery. The two together can help you more than surgery alone.
Goals of surgical repair for Pelvic Organ Prolapse
Goals of surgery include improving urinary, bowel and sexual symptoms or keeping symptoms from getting worse. Goals also include supporting pelvic structures, preventing new symptoms and preventing prolapse from coming back. Good habits for your lower belly must be developed before surgery and continued after surgery to prevent prolapse from coming back. The need for repeat surgery in pelvic organ prolapse may be as high as 30%.
Surgeries for Pelvic Organ Prolapse
Treatment options include closing the vagina or restoring normal position of pelvic organs.
Closure of the vagina (colpocleisis) is one of the least invasive surgeries for pelvic organ prolapse. Patients can no longer have sexual intercourse after surgery. Patients who chose closure of the vagina tend to be older and have other medical problems that make invasive surgery more difficult. One study showed an average age of 77 years old. The success rate is 90% to 100% with a low complication rate. The patient satisfaction rate is greater than 90%.
Surgery to restore normal position of the Pelvic Organs
Surgery to restore the normal position of the organs can be performed through the vagina or through the abdomen. Goals of surgery are placing the vagina back to normal position and maintaining normal length and function.
Vaginal Surgery
Prolapse can be treated through the vagina by attaching the top of the vagina to ligaments inside the lower belly. Advantages of surgery through the vagina are decreased operating time, recovery time and cost. Surgery through the vagina also avoids the recovery time needed for an incision in the belly. Disadvantages may be a higher rate of prolapse coming back.
Abdominal Surgery
Open Sacrocolpopexy – This surgery is performed through an incision in the low belly. Mesh is used to recreate the natural support of the vagina (uterosacral and cardinal ligaments). One end of the mesh is attached to the top of the vagina or cervix. The other end of the mesh is attached to the front of the spine (sacral promontory). This puts the vagina back in its normal position and provides support. The length of the vagina remains the same, which is important in patients who are still sexually active. Use of mesh provides a source of strength in patients whose own tissue is weak. Overall, open sacroculpopexy has a 78% to 100% long-term success rate for the treatment of prolapse.
A recent review of 40 studies compared vaginal surgery (sacrospinous ligament suspension) to open abdominal sacroculpopexy. Abdominal sacroculpopexy resulted in a better repair of prolapse, lower rate of prolapse coming back and less pain during sex than vaginal repairs.
Another study compared vaginal surgery (bilateral sacrospinous fixation) to abdominal sacroculpopexy after two and a half years and found the abdominal sacroculpopexy group was twice as likely to have an good outcome and 50% less likely to require repeat surgery (Benson et al 1996). Prolapse came back in 2.6% of people in the abdominal sacroculpopexy group versus 12% of people in the vaginal (sacrospinous) group.
The disadvantages to open abdominal sacroculpopexy compared to vaginal surgery are increased surgery time, recovery time and cost.
Laparoscopic sacrocolpopexy – This surgery offers a less invasive approach to the repair of prolapse along with smaller scars. This approach provides an improved view to the surgeon during the procedure. Advantages of this minimally invasive approach are less pain after surgery, less blood loss and a shorter length of hospital stay.
The major disadvantages are that the technique is difficult to learn and surgery typically takes more time than open abdominal surgery.
Robotic sacrocolpopexy – The da Vinci® surgical robot was approved by the Food and Drug Administration in 2005 for use in gynecologic surgery. Compared to laparoscopic surgery, the da Vinci robotic surgical system offers a 3-dimensional picture, magnification, easier instrument movement and a wider range of movement. This makes complicated surgical tasks easier to perform.
Advantages of the robotic sacroculpopexy compared to the open abdominal sacroculpopexy are less blood loss, shorter hospital stay and smaller scars.
Disadvantages are longer surgery time and higher cost.
Supracervical hysterectomy – If the uterus is also involved in the prolapse, a hysterectomy can be performed by a gynecologist at the time of the prolapse repair.
Supracervical hysterectomy removes the uterus and leaves the cervix in place. Leaving the cervix in place leaves more tissue behind to attach the mesh and can decrease the risk of mesh erosion.
The chance of developing cancer in the remaining cervix has been reported as low as 0.11% and 0.2%. With continued screening Pap smears, the risk of cervical cancer is < 0.1%. Therefore it is important to continue screening Pap smears with your gynecologist if the cervix is left in place.
Complications
Studies have shown no difference in the rate of complications between open versus laparoscopic surgery.
Early complications include injury to pelvic structures (bowel, bladder, ureters or kidney tubes), infection, blood clot formation, bleeding and slow return of bowel function. The risk of bladder injury during abdominal sacroculpopexy ranges from 0.4% to 15.8%.
Other complications that can occur any time are new leakage of urine with cough (15%), overactive bladder (12%) and other problems urinating not present before surgery (12%). Sometimes surgery for leakage of urine is performed at the time of robotic sacroculpopexy.
Complications after surgery include bowel blockage (1.1%), mesh erosion (3.4%) and hernia (5%).
Summary
Multiple treatment options exist for the management of vaginal vault prolapse. Each has their own advantages and disadvantages. Robotic sacroculpopexy is a minimally invasive surgery that has a high success rate for treatment of prolapse with a long-lasting result.
Additional information
Contact us to request an appointment or ask a question. We're here for you.



