Urinary Tract Infection in Women
Recurrent cystitis is a term use to describe repeated bladder infections. This is a common condition which affects woman of all ages. It is estimated that approximately 80% of women will acquire a bladder infection at some time during their life. As many as 20% of women will have problems with recurrent infection.
The function of the urinary tract is to clean waste products from the blood. The urinary tract begins with the kidneys which sit high in the back. Blood is filtered through the kidneys which extract excess fluid and waste products to make urine. Once the urine is made by the kidney, it is carried down through tubes called “ureters” to the bladder.
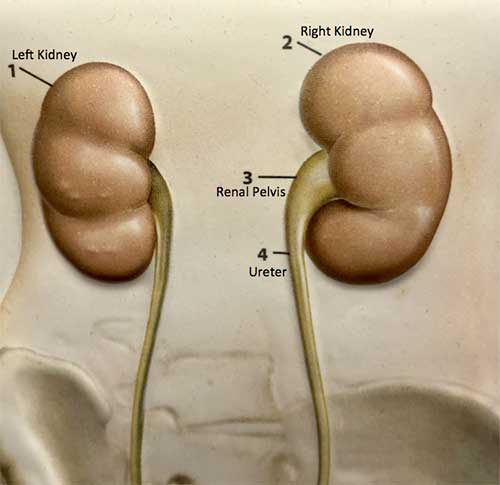
The bladder sits in the pelvis, which is in the area in the lower abdomen. The bladder stores urine until full then empties the urine to the outside through the urethra.
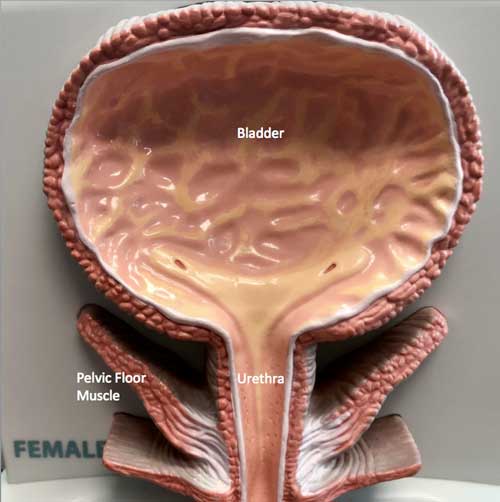
Infection in the urinary tract can occur when bacteria gain access to the bladder. Bacteria are normally present at the bladder opening or “urethra” and in the vagina, which is just below the urethra.
These bacteria can ascend up through the urethra to reach the bladder. Once present in the bladder, the bacteria can multiply and produce infection.
Symptoms
The typical symptoms of bladder infection are frequent urination, painful urination, and urgency – the feeling of the need to urinate right away. Lower abdominal or pelvic pain may be present. Another symptom may be a sense of feeling the need to urinate again, in spite of having just emptied the bladder. Low grade fever and low back pain may be present.
Diagnosis
The diagnosis of infection begins with a history and physical exam. A urinalysis may be performed to determine if white blood cells (or pus cells) or blood may be present. The urine may be sent to the lab for a microscopic examination and culture. A urine culture determines if there are bacteria in the urine which can be grown in the laboratory. If bacteria grow, the bacteria responsible for the infection can be identified. This allows selection of the appropriate antibiotic treatment. Urine study should be obtained before starting treatment for each episode of infection.
Treatment
Treatment of bladder infection begins with antibiotic therapy. Antibiotics are given for a period of time varying time, often from one to seven days. Antibiotics should be given for a short duration as is reasonable to avoid excess antibiotic exposure. First-line antibiotics include nitrofurantoin (Macrobid), trimethoprim–sulfamexoxazole (Bactrim) and fosfomycin (Monurol). In addition to antibiotics, increased fluid intake is recommended. Increased fluid causes the kidneys to produce more urine. When more urine is produced, the bladder fills more frequently and empties more often. More frequent emptying of the bladder helps to “wash out” infection from the bladder.
Urinary acidification can help prevent recurrent infections. Cranberry juice or pills or vitamin C acidifies the urine, which produces a less favorable environment for bacteria. Probiotics promote growth of healthy bacteria and makes it harder for bacteria to stick to the urinary tract.
Recurrent Infections
For women who develop recurrent infections, the usual cause is repeated episodes of bacterial infection of the bladder. There is a common misperception that recurrent bladder infection is due to an inadequately treated infection. However, repeat infection is usually due to a new episode of infection which occurs once the previous one has been treated.
Risks for recurrent urinary tract infection
Several recognized initiating events can trigger infection. Sexual intercourse is a risk for bladder infection. It appears that the pressure in the vaginal area which occurs at intercourse may facilitate ascent of bacteria up the urethra into the bladder. Some women report that they develop bladder infection almost every time that they have intercourse. New sexual partners and barrier methods of contraception (condoms, spermicide, diaphragm, cervical) are additional risk factors for bladder infection. Bowel dysfunction, including diarrhea and constipation, are also risk factors for recurrent infection.
Evaluation
For women who have recurrent infections, the urinary tract is often evaluated by a urology provider to determine if there is an underlying abnormality. A medical history is obtained. Pelvic examination may be performed. Urine may be studied by urinalysis or "dipstick" in the office. Urine may be sent out to the laboratory for microscopic exam and culture. If microscopic examination of the urine shows skin cells (epithelial or squamous cells), the test may not be accurate. A repeat urine test may be performed in the office for a “catheterized sample”. A small plastic tube called a “catheter” is passed through the urinary opening into the bladder. This allows collection of urine directly from the bladder and bypasses the skin of the urinary tract. This is more accurate way to check the urine if the interpretation initial clean catch urine sample is unclear.
An assessment can be made of the degree of bladder emptying. A post-void residual is checked, which is the amount of urine left in the bladder after urinating. This is done to determine if the bladder empties completely or if it retains a large volume of urine. Incomplete bladder emptying is a risk for recurrent infection. This is performed by ultrasound in the office after emptying the bladder.
Supplements may be added to decrease the risk of urinary tract infection. See below.
If a woman has a history of kidney stones or other urinary tract problems, further studies may be performed. Ultrasound of the kidneys and bladder may be performed to determine if kidney stones, blockages or other abnormalities are present. The bladder may be examined with cystoscopy. A small thin fiberoptic camera is placed through the urethra into the bladder to exam in the urethra and bladder. The urologist can inspect the bladder lining to make sure that there are not any intrinsic problems within the bladder itself. This study can identify out bladder stones, abnormal anatomy, bladder tumors, ulcers, urethral pouches or scarring. This study is typically performed in the office. If any abnormalities in urinary tract are identified on these studies, appropriate treatment is carried out.
Urinary Tract Infection Prevention
Bladder hygiene
- Drink at least 2 liters (60 ounces) of fluid per day. Fluids dilute and flush out bacteria. Water is best. Increase water intake until urine is clear light yellow.
- Empty the bladder frequently, never hold the urine more than 3 to 4 hours. This decreases the amount of time bacteria stays in the bladder.
- Wipe front to back to decrease the amount of bacteria near the urinary opening (urethra).
- Eat a high-fiber diet. Constipation can make it difficult to empty the bladder well and can increase risk for UTI. Diarrhea can increase genital exposure to bacteria. May use 2 tablespoons of flaxseed powder daily.
- Barrier methods of contraception (condoms, spermicide, diaphragm) are risks for UTI. Spermicides change the vaginal environment and can increase vaginal bacteria. Use a different methods for contraception if possible.
Supplements
- Cranberry
Cranberry decreases the ability bacteria to stick to the bladder lining. Use twice daily. May use juice or pills (egTheraCran). Take pills if diabetic or juice causes stomach upset. Use low sugar juice if diabetic or overweight. - Probiotic
Probiotics maintain healthy gut bacteria and makes it more difficult for bacteria to stick to the bladder lining and grow. Take at least 5 billion units of lactobacillus acidophilus daily. May also use yogurt, kombucha, kefir, intravaginal probiotic. - D-mannose
D-mannose is a sugar that decreases ability of bacteria to stick to the bladder lining. May use pills or powder (2 grams in 200 mL of water). Take daily. - Vitamin C (ascorbic acid)
Vitamin C makes the urine more acidic so it is harder for bacteria to stick to the urinary lining. Take 500 mg once or twice per day. Do not use if you have history of kidney stones. (Vitamin C is converted to oxalate and excreted in the urine. It can increase the risk of calcium oxalate stones.) - Methanamine (eg Cystex)
Methanamine has antiseptic properties that make it harder for bacteria to stick to the bladder lining. Methanamine works best in acidic urine. A urine pH of 5.5 or less is best. Take methanamine with vitamin C for best results. Urine test strips can be purchased over-the-counter or online to monitor your urine acidity (pH).
Prescription
Non antibiotic
Used in women in menopause to increase normal healthy lactobacillus bacteria in the vagina. This make it harder for bacteria that cause infection to enter the bladder. Use before bed 2 to 3 nights per week. This can cause vaginal irritation in about 20% of women. Estrogen pills by mouth do not help prevent UTI.
Methanamine acidifies the urine and makes it more difficult for bacteria to stick to the bladder lining.
Before you start taking this medicine, urine needs to be checked with phenaphthazine paper (urine test strip) or another test to see if it is acid. This can be done in the office or at home. The urine must be acidic (pH 5.5 or below) for this medicine to work properly. If you have any questions about this, talk to one of our providers.
The following changes in your diet may help make your urine more acid; however, check with your doctor first if you are on a special diet (for example, for diabetes). Avoid most fruits (especially citrus fruits and juices), milk and other dairy products, and other foods that make the urine less acid. Also, avoid antacids unless otherwise directed by your doctor. Eating more protein and foods such as cranberries (especially cranberry juice with vitamin C added), plums, or prunes may also help. If your urine is still not acid enough, check with your doctor. If this medicine causes nausea or upset stomach, it may be taken after meals and at bedtime.
Do not use if low kidney function. Liver and kidney function should be monitored if used for more than 3-6 months.
Antibiotic
Sexual intercourse is risk for infection. An antibiotic pill may be taken immediately before or after intercourse to prevent infection from developing. This is useful for patients who develop recurrent infection after intercourse.
A prescription may be given to have antibiotics on hand. Many women can tell when they develop an infection. A course of antibiotics are started at the onset of symptoms. Urine studies including urinalysis, microscopy and culture should be checked before starting treatment for each episode of infection. These studies give information about the composition of the urine, bacterial growth, type and quantity of bacteria and what antibiotic will treat the infection. Urine can be checked at the urology office, a primary care doctor or urgent care to check urinalysis and send out for microscopy and culture. Home urine test strips can be purchased over the counter without a prescription. This serves as a screening urinalysis. If a home urine test strip is abnormal, urine should be checked in the office.
Patients take their antibiotic for a one to five day period once symptoms develop. This usually clears the infection. If symptoms persist beyond that point, then it is time to check in with a healthcare provider.
The philosophy of this regimen is that the antibiotics are much more effective when the infection first begins than when they are used after infection has been present for several days.
A patient takes a low dose of an antibiotic once a day before bed for a period of several months in order to keep the bladder free of infection.
Contact us to request an appointment or ask a question. We're here for you.




