Elevated PSA - Prostate Cancer Screening
More Info from American Urological Association:
Is Prostate Cancer Screening Right For You?
How does the urinary system work?
The urinary tract begins with the kidneys. The kidneys, one on each side, sit high in the upper abdomen partially underneath the rib cage. They filter the blood to extract excess waste products and fluid to form the urine. Urine, once formed in the kidneys, travels through a tube on each side, the ureter, down to the bladder.
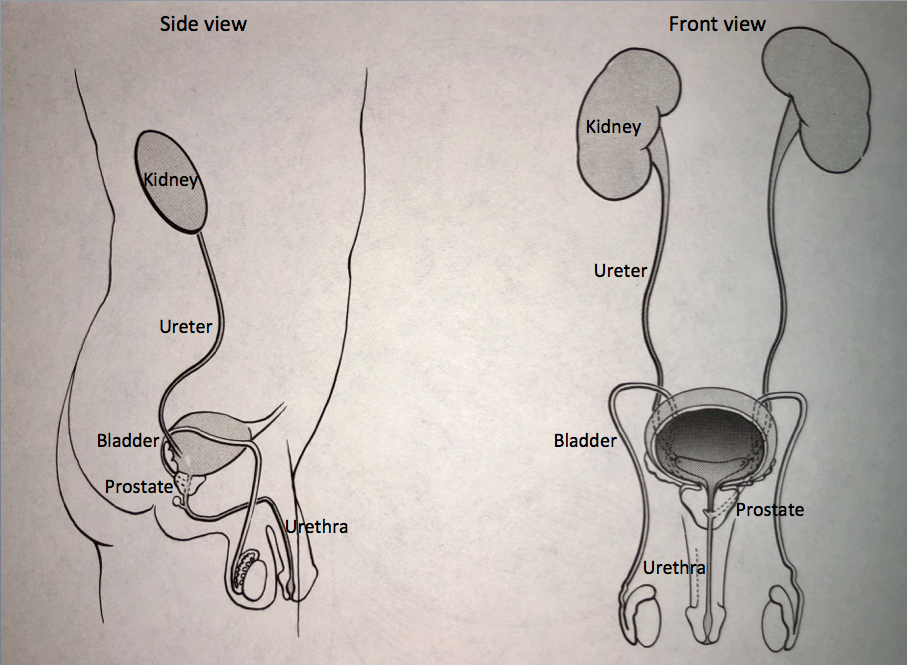
Urine is constantly being made by the kidneys and transported through the ureters into the bladder. The bladder stores urine until full and then empties to the outside through the urethra. The prostate, which is a gland that is part of the reproductive system, forms the first part of the urethra.
What is the prostate? How does it change over time?
The prostate is a gland which is part of the reproductive system. It makes a portion of the semen, which is the fluid that comes out at the time of ejaculation. The prostate forms the first part of the urethra which is the urinary channel that drains urine from the bladder to the outside through the penis.
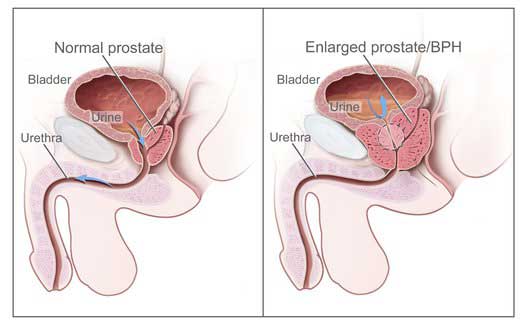
The prostate begins to enlarge in a benign or non-cancerous fashion (called Benign Prostatic Hyperplasia or BPH) in almost all men beginning at the age of 40. As it does, it can block the urinary channel and may cause a change in the pattern of urination.
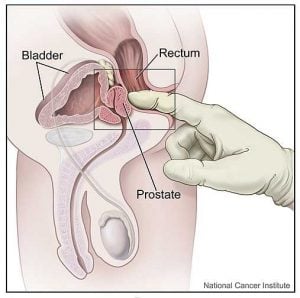
While normal growth of the prostate affects most men, approximately 1 out of 10 men will develop cancer of the prostate. Currently, men are checked for prostate cancer with a digital rectal exam (DRE) and a PSA blood test. A digital rectal examination is an exam carried out by a doctor where a gloved finger is inserted into the rectum to palpate the prostate for abnormalities that may suggest the presence of cancer.
What is PSA?
PSA, which stands for prostate specific antigen, is a protein made only in the prostate and not elsewhere in the body. Since the 1990’s, PSA has been routinely used as a test to screen for prostate cancer.
PSA is not specific for prostate cancer. There are actually three common conditions which cause PSA elevation: BPH, prostatitis and prostate cancer. BPH or Benign Prostatic Hyperplasia is the normal enlargement of the prostate that occurs in most men once they reach the age of 40. Prostatitis, which is nonspecific inflammation of the prostate, is another common cause of PSA elevation and likely affects 1 out of 4 men.
What is a normal PSA? Are there tests which can increase its usefulness to check for prostate cancer?
Traditionally, PSA has been considered to be normal between 0 and 4. However, there are a number of factors that need to be considered when evaluating a man’s PSA, such as age and trend of PSA over time.
An important feature of PSA appears to be its rate of change over time, referred to as “PSA velocity.” For those men with BPH or prostatitis, the PSA may vary several points a year but it tends to stay the same range over time. For those men with prostate cancer, the PSA tends to have a steady rise and levels can increase by as much as to 100% on a yearly basis.
The level of PSA can also be correlated to the size of the prostate. The “PSA density” is the value of PSA divided by the size of the prostate measured at the time of the prostate ultrasound. If the PSA is higher than expected for that size prostate, then there may be an increased possibility that prostate cancer may be present.
Another variation of PSA testing is known as “free versus total” PSA. A portion of the PSA in the bloodstream is bound to a carrier protein and the remainder is unbound or “free.” The ratio of the free versus total PSA may be useful to help determine if PSA elevation is due to BPH or prostate cancer. If the % free is near 10%, there is increased concern that cancer may be present.
Different PSA levels have been established for different age groups. PSA ranges according to age are as follows:
| Age | PSA Levels |
|---|---|
| 41-50 | 0.0-2.5 |
| 51-60 | less than 3.5 |
| 61-70 | less than 4.0 |
| Over 70 | less than 6.5 |
It should be noted that in some men, there may be a slight increase in PSA within 48 hours after ejaculation, and current recommendations are that men wait 48 hours after ejaculation before PSA value is checked.
If there is concern that the elevated PSA may be due to prostate cancer, what is done to see if cancer is present?
When PSA is elevated, the next step depends on the degree of elevation and the health status of the patient. Recommendations may include serial PSA monitoring, additional types of blood tests that check sub types of PSA or imaging with prostate MRI.
Prostate MRI
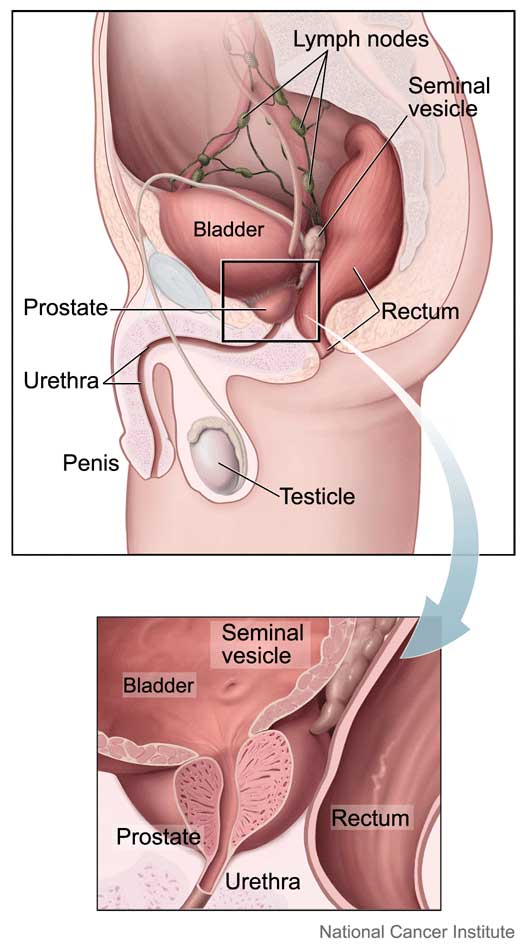
In 2020, the American Urological Association released to statement supporting the use of prostate MRI before biopsy. Traditional transrectal ultrasound-guided biopsies involved random sampling of the prostate. Prostate MRI visualizes the entire prostate and surrounding anatomy including the glands behind the prostate (seminal vesicles), lymph nodes and bony structures. Prostate MRI can also show abnormal areas in the prostate. When there is an abnormal area, the radiologist reports the size, location and how worrisome the lesion is for cancer.
PI-RADS scoring system for prostate MRI
PI-RADS is a scoring system developed by radiologists to note how worrisome an MRI prostate lesion is for cancer. PI-RADS stands for Prostate Imaging-Reporting And Data System. The scoring system ranges from 1-5. The lesion with a score of PI-RADS 1 has a very low risk for significant prostate cancer is present. A lesion with a PI-RADS 5 score is a very high risk for significant prostate cancer is present. The PI-RADS score helps determine the likelihood biopsy is needed.
MRI fusion prostate biopsy
If the prostate MRI shows worrisome areas, MRI fusion prostate biopsy may be recommended. This technology combines live transrectal ultrasound with MRI prostate images. This allows targeted biopsies of the prostate lesions seen on MRI. It has been shown to improve the detection of worrisome prostate cancer. It has also been shown to decrease biopsies of slow-growing insignificant cancer. MRI fusion prostate biopsy is performed in an outpatient setting with IV sedation. An ultrasound probe is placed in the rectum. Specialized software allows mapping of the prostate MRI with the live ultrasound images. Typically 2-3 biopsies are taken from each lesion identified on MRI. Approximately 12 standardized biopsies are taken of the remaining prostate.
Transrectal Ultrasound (TRUS) of the prostate
If there are no lesions on prostate MRI at the PSA is still elevated, transrectal ultrasound and prostate biopsy may be recommended. Transrectal ultrasound (TRUS) of the prostate is an imaging technique that provides a complete view of the prostate, allowing visualization of areas which cannot be felt on a digital rectal examination. TRUS is carried out in the outpatient setting with IV sedation (similar to a colonoscopy). An ultrasound probe is placed in the rectum.
The size of the prostate can be measured. The prostate is inspected for irregularities of contour. Ultrasound typically does not identify any areas that stand out as “suspicious for cancer”. The main value of ultrasound imaging of the prostate is that it allows very precise, systematic, grid-like, step-by-step sampling (biopsy) of the prostate.
As many as 16 or more biopsies of the prostate are taken. These “core” samples are almost an inch long and extend from the back of the prostate through to the front. A needle, which is the same size as a needle used to take a blood test in the arm, is used to take the samples of the prostate.
It is this orderly, sequential sampling that provides the most effective approach to determine if prostate cancer is present.
Risks of prostate biopsy
Complications are rare after biopsy of the prostate but include bleeding and infection. To minimize the risk of bleeding, patients are instructed to stop all aspirin or aspirin like compounds seven to ten days prior to the procedure. Patients who are taking a blood thinner, (i.e. Coumadin) need to stop the medication five days prior to the procedure. To minimize the risk of infection, preventive antibiotics are given the day before, the day of and the day after the procedure. A Fleets enema is usually given the day of the procedure to empty the rectal area.
Follow up
For patients who undergo prostate biopsy and have benign findings, we recommend careful, ongoing follow up. Patients should have a follow up digital rectal exam and PSA approximately six months after their procedure and at regular six months intervals thereafter.
Do all men with prostate cancer need treatment?
The standard of care to evaluate an elevated PSA has been prostate ultrasound and prostate biopsy which has led to a marked increase in the number of men diagnosed with prostate cancer.
Of all those men who are diagnosed with cancer, a subset will have aggressive type of the disease that if left untreated, will progress with cancer spread beyond the prostate and which may eventually cause death from prostate cancer.
With the recognition that some men have low risk type of prostate cancer that will not require treatment, controversy exists for PSA screening because it can lead to over diagnosis and over treatment of prostate cancer. Additional tools are now available to improve risk assessment prior to prostate biopsy, which can be used in an effort to reduce the number of prostate biopsies performed, to reduce the diagnosis of low grade prostate cancer, and to still offer the opportunity to identify high-grade cancers. New blood tests have been developed to help guide that selection process include the 4K test, which looks at sub units of PSA, which can potentially identify those men who may have a more high risk form of prostate cancer, for which prostate cancer treatment would be indicated.
At what age is PSA no longer needed?
The AUA guideline panel does not recommend routine PSA screening in men over age 70 or any man with a less than 10 to 15 year life expectancy. Some men age 70 and above, who are in excellent health with a life-expectancy over 10 to 15 years, may benefit from prostate cancer screening but there is strong evidence that the ratio of harm to benefit increases with age and that the likelihood of over diagnosis is extremely high particularly among men with low-risk disease. In order to identify the older man more likely to benefit from treatment if screening takes place, the panel recommends two approaches: 1) increasing the prostate biopsy threshold (e.g., PSA above 10); and 2) discontinuation of PSA screening among men with a PSA below 3.
Take Home Message
We have been using PSA in combination with trans rectal ultrasound guided biopsy since 1991. Prior to that time, prostate cancer was typically diagnosed once it had already spread from the prostate, in which case treatment was less effective. With the onset of the “PSA era”, we have diagnosed prostate cancer in many of our patients. We offer the encouraging news that we can attempt to identify those prostate cancers that need treatment, and if so, we have the opportunity to diagnose them at an early stage, when the cancer may still be confined within the prostate and not spread, which is the stage at which prostate cancer is most curable.
Contact us to request an appointment or ask a question. We're here for you.


